Treatment Overview for Breast Cancer
If you have breast cancer or are at high risk for breast cancer, you’ve come to the right place. We’re here to help you with the decision-making process and guide you through your breast cancer treatment journey.
Treatment
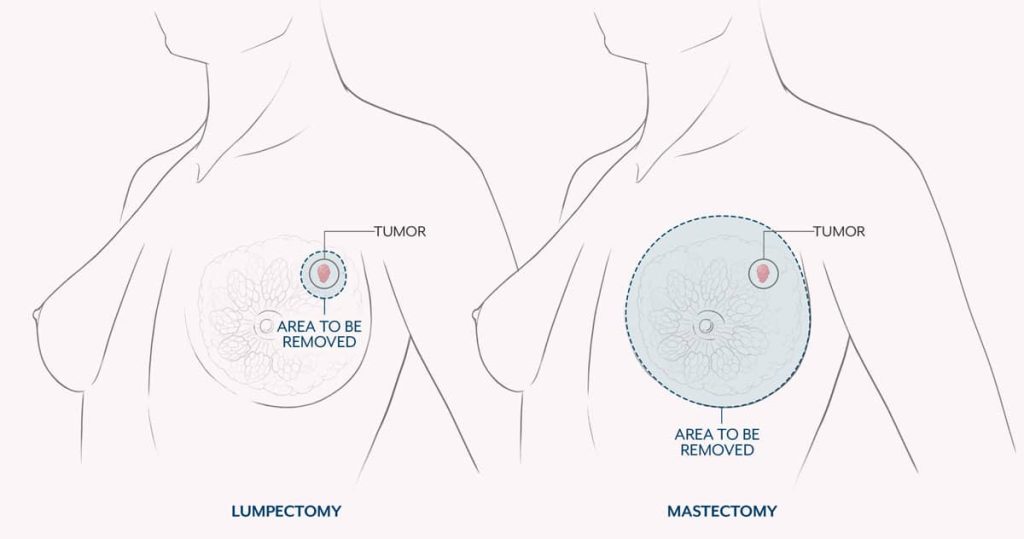
Surgery to remove breast cancer is the most common form of treatment after a diagnosis. Surgery options include a mastectomy (removal of the breast) and lumpectomy (removal of the breast tumor and surrounding tissue).
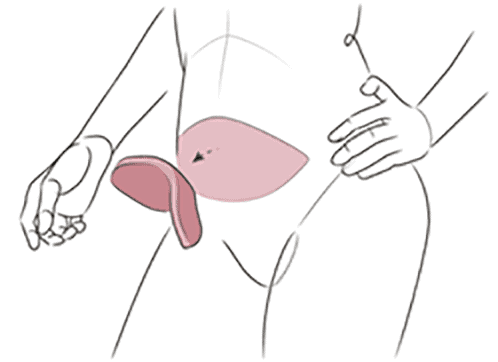
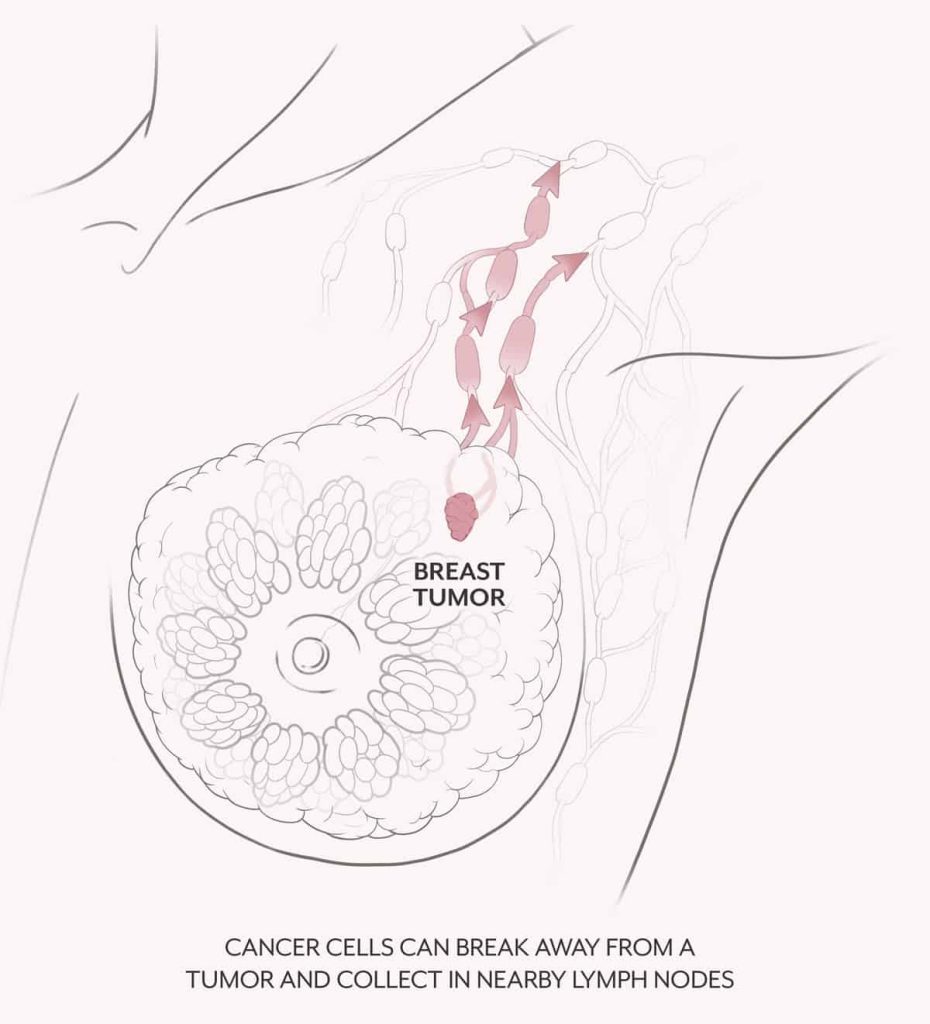
In some cases, women also need to have lymph nodes removed as part of their cancer surgery. Breast cancer can move from the breast to the chain of lymph nodes in the armpit region. Those lymph nodes are a component of your body’s lymphatic system, which helps your body fight infection as well as remove toxins and debris. The lymphatic system drains into lymph nodes in several areas in your body. Cancer cells from a breast cancer tumor can break off and travel through the lymphatic channels into lymph nodes.
Determining whether the axillary lymph nodes contain cancer will help your doctor determine what additional breast cancer therapy, such as chemotherapy and radiation therapy, is needed to treat the breast cancer.
The first lymph node in the chain is called the “sentinel” lymph node. To identify the sentinel lymph node, your surgeon will inject a dye or radioactive tracer into the breast at the time of surgery. This dye or tracer is taken up in the lymphatic system and migrates to the lymph nodes. Identifying and removing the sentinel node allows your surgeon to correctly “stage” your cancer and see if there is any sign of spread to the lymph nodes. This procedure is called a sentinel node biopsy.
If the sentinel node has no tumor cells, it is unlikely that lymph nodes further up the chain will have tumor cells. If cancer cells are found in the sentinel node, then additional lymph nodes may be removed. This procedure, known as axillary dissection, also takes place during your cancer surgery and helps guide your cancer team’s future treatment planning.
Axillary dissection removes approximately 10-20 lymph nodes and allows your surgeon to stage your cancer with a high degree of accuracy. This procedure is typically only done when multiple abnormal nodes can be felt, when nodes have not gone away following treatment administered before surgery, or in cases of inflammatory or recurrent breast cancer.
In some cases, women also need to have lymph nodes removed as part of their cancer surgery. Breast cancer can move from the breast to the chain of lymph nodes in the armpit region. The first lymph node in the chain is called the “sentinel” lymph node and can be identified by injecting a dye or radioactive tracer into the breast at the time of surgery. This dye or tracer is taken up in the lymphatic system and migrates to the lymph nodes. By identifying and removing the sentinel node, your surgeon can see if there is any sign of spread to the lymph nodes. If the sentinel node has no tumor cells, it is unlikely that lymph nodes further up the chain will have tumor cells.
If cancer cells are found in the sentinel node, then additional lymph nodes may be removed. This procedure, known as axillary dissection, also takes place during your cancer surgery and helps guide your cancer team’s future treatment planning.
Axillary dissection may cause swelling in the arm due to impairment of the lymphatic drainage from the arm. This swelling is called lymphedema. The Friedman Center also offers an innovative lymphatic surgery called LYMPHA, which is done at the same time as a lymph node removal, to help prevent lymphedema. The extent of your cancer, the size and shape of your breasts, and your personal preferences will help determine which of these surgeries may be right for you.
In some cases, breast cancer surgery is combined with other treatments, such as chemotherapy, targeted therapy, and radiation therapy. Treatments given after surgery are called “adjuvant” treatment; when they are given before surgery, they are called “neoadjuvant” treatment. Your team of physicians will work together to build a customized treatment plan with you and make sure you understand all your options.
Additionally, most women diagnosed with breast cancer are candidates for breast reconstruction surgery. A plastic surgeon, like our physicians at the Friedman Center, can review your options for reconstruction. We recommend consulting with a plastic surgeon even if you consulting with a plastic surgeon.

Breast cancer surgery and treatment may involve multiple
specialties. It is important that you feel confident in your treatment
plan and comfortable with your team of healthcare specialists.

Learning to ask questions about your options can empower you
to make the right decisions for you.
Things to think about and discuss with your surgeon:
Should I have a lumpectomy or mastectomy?
What are the characteristics of my particular type of breast cancer?
Do I need additional cancer treatment beyond surgery?
Can breast reconstruction be done at the same time as a mastectomy?
Will cancer treatment impact the timing of my breast reconstruction?
Do I need any lymph nodes removed?
What is lymphedema and how can I prevent it?
Who will be on my breast care management team?
How can I best prepare myself for breast cancer surgery?
Nationally recognized for excellence in cancer care
The Friedman Center partners with the Northwell Health System, whose hospitals and cancer programs are nationally recognized for excellence and accredited by leading organizations in cancer care, including the National Accreditation Program for Breast Centers (NAPBC).
This accreditation means that we have voluntarily gone through a rigorous peer review process to ensure we meet nationally accepted standards, have well-qualified staff to diagnose and treat your cancer, and employ technology that meets or exceeds guidelines so that you receive the safest, highest quality care. Learn about Northwell Health’s cancer programs here.