About Breast Reconstruction
Breast reconstruction is surgery done to rebuild the breast. The goal of breast reconstruction is to recreate the look and feel of the natural breast, create symmetry between the two breasts, and restore the nipple and areola. For many women, having breast reconstruction after a mastectomy or lumpectomy is vital to restoring their confidence and self‑identity.
For women who have breast cancer or are at high genetic risk for breast cancer, surgery is often part of their treatment or prevention plan. Mastectomy and lumpectomy procedures remove all or some of the breast tissue; through breast reconstruction, a woman’s breasts can be recreated.
Breast reconstruction is performed by a plastic surgeon who is usually highly trained in advanced microsurgery. Reconstruction may happen at the same time as a lumpectomy or mastectomy (immediate reconstruction), or it can occur as one or more separate procedures at a later date (delayed reconstruction).
A Personal Choice
The decision to have breast reconstruction is very personal, and may not be right for every woman. Many women find that restoring the breast helps them feel complete and whole again, lessening the psychological and emotional impact of a mastectomy or lumpectomy. Other women opt not to reconstruct their breasts, choosing to “go flat“ instead.
We’re here to offer guidance and education about the available options so that you can make an informed and empowered decision about breast reconstruction.
To learn more about the breast reconstruction process, see What to Expect from Diagnosis to Recovery.
About Breast Reconstruction Overview
After lumpectomy or mastectomy, you may decide to have breast reconstruction as part of your treatment plan. The following video describes several options that you might consider.
Types of Breast Reconstruction
The most common approaches to breast reconstruction are implant reconstruction and natural tissue reconstruction (also known as flap reconstruction). Hybrid reconstruction, which combines both implant and tissue flap methods, may be used in some cases. Finally, partial breast reconstruction is an alternative for women who have had a lumpectomy.
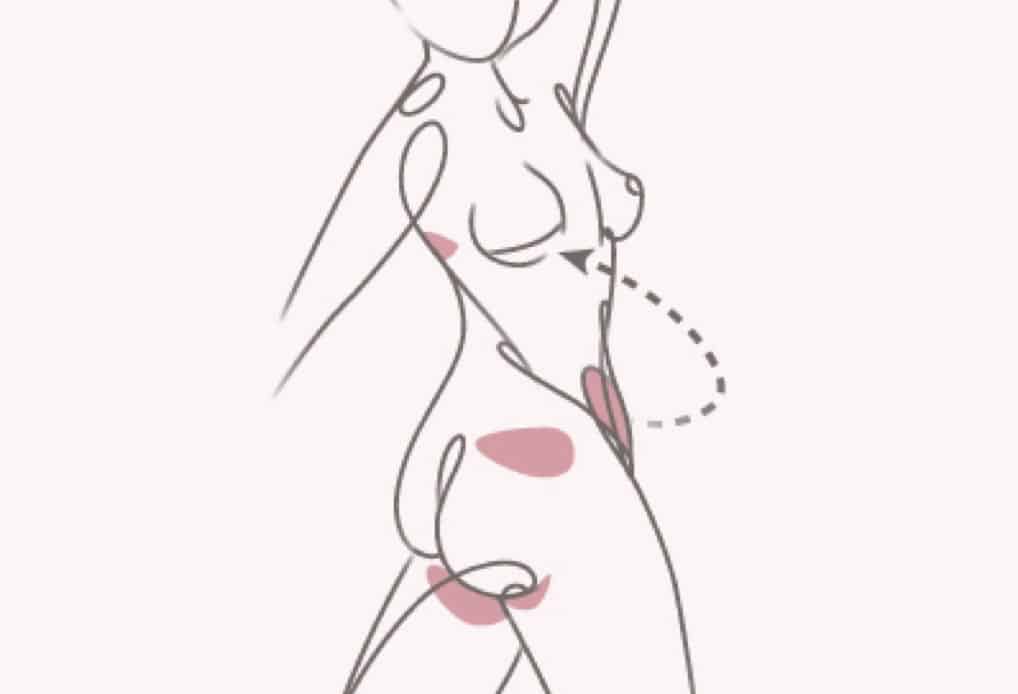
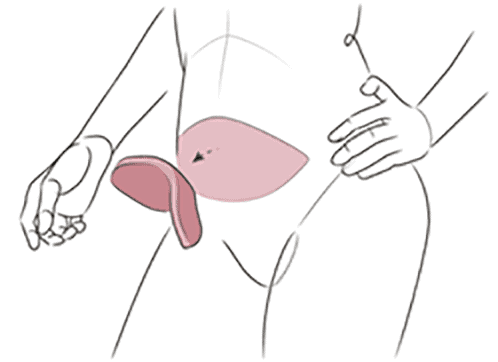
This type of breast reconstruction uses tissue from your own body to form the new breast. A flap of tissue is taken from one part of your body, along with its blood supply. That helps the tissue flap survive in a new location and allows it to be used for reconstruction. Tissue flap procedures typically either leave the tissue partially attached, or they detach and then reconnect small blood vessels to restore circulation. The surgeons at the Friedman Center specialize in the DIEP flap procedure, considered the gold standard of natural tissue breast reconstruction. Some women may also be eligible for groundbreaking robotic surgery techniques.
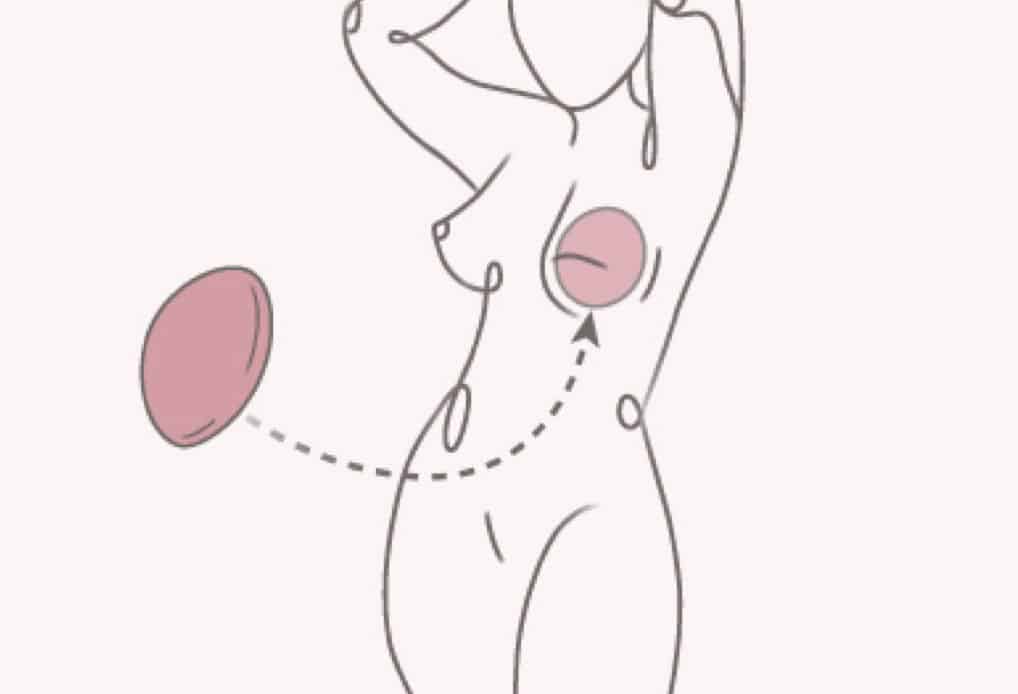
In this type of reconstruction, a synthetic implant containing saline solution or silicone gel is surgically inserted to form the shape of the new breast. Implants come in many different shapes and sizes, and they are a very common method of restoring the breast after breast cancer. This technique may use an adjustable temporary implant prior to placing the final implant. This allows for proper healing and helps patients choose the best size long term.

Which type of reconstruction is right for you?
Compare natural tissue and implant reconstruction
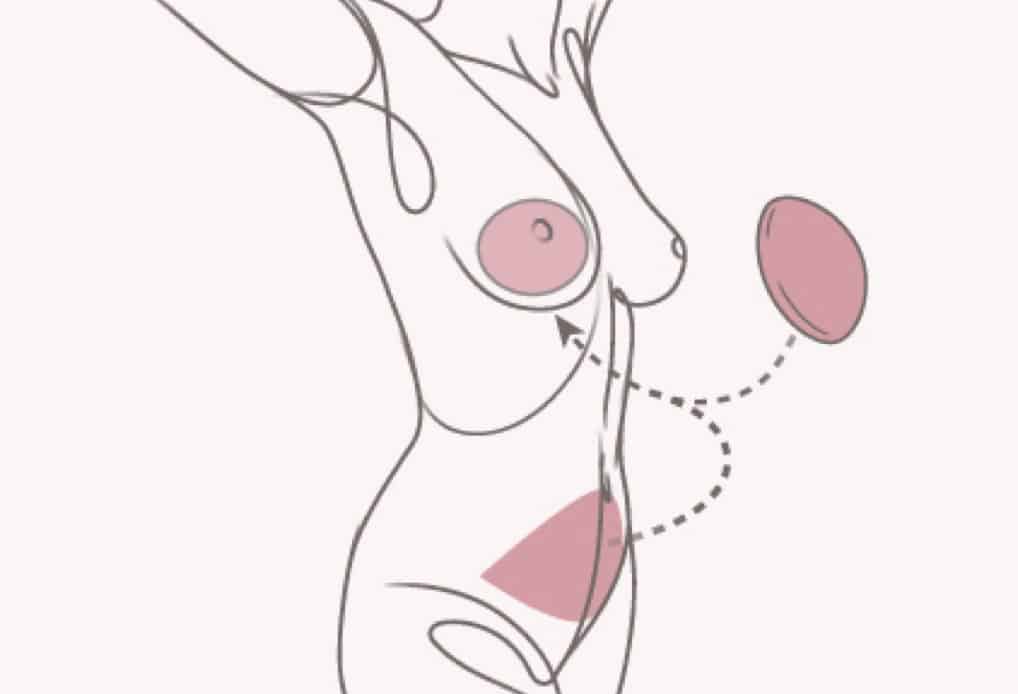
Hybrid reconstruction uses both tissue from your own body and a synthetic implant to rebuild the breast. The hybrid approach may be a viable option for women who may not see optimal results from flap or implant reconstruction alone.

Partial reconstruction recreates symmetry in the breasts after a partial mastectomy, also known as a lumpectomy. There are several possible approaches to this type of reconstruction, including breast lifts or reductions, tissue transfer, fat grafting, or implants.
The Friedman Center is now performing robotic surgery for DIEP flap procedures.
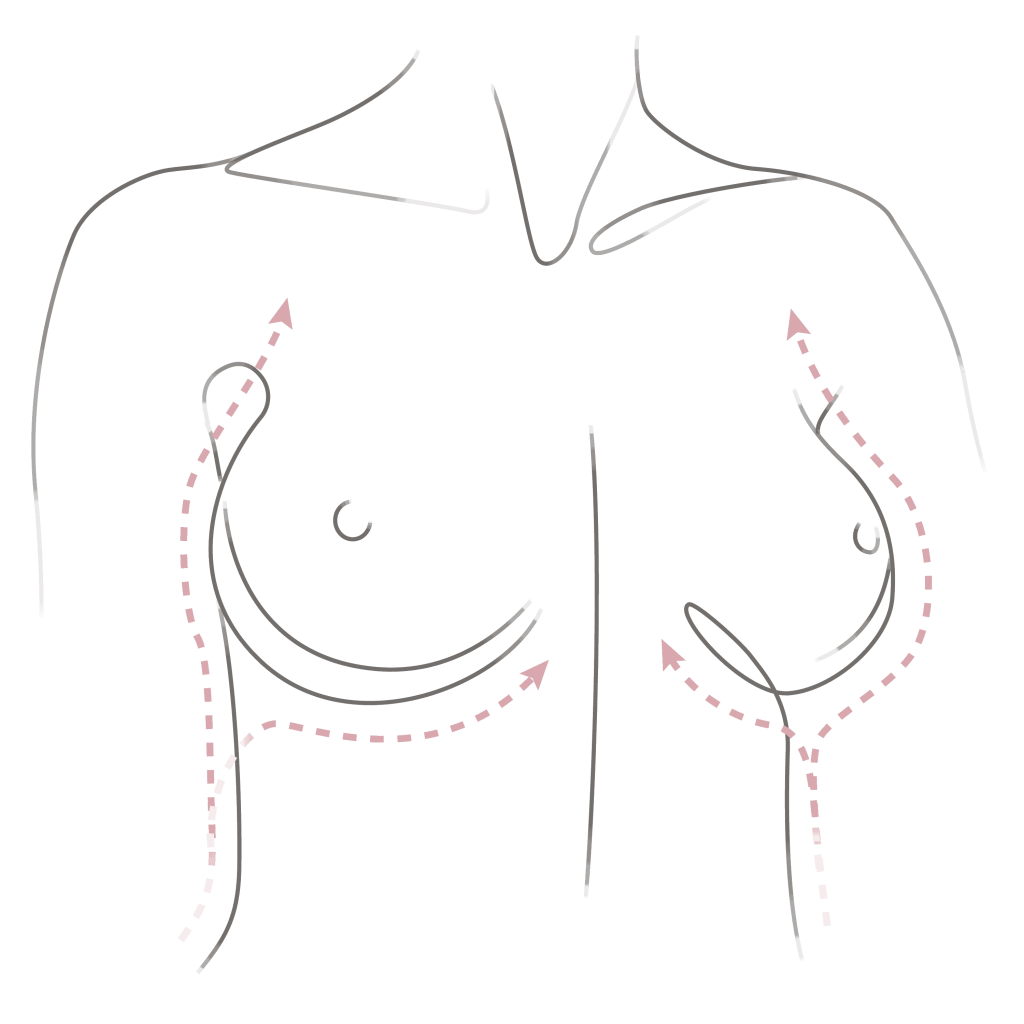
If you are having a single mastectomy, you may also wish to have cosmetic surgery on the opposite breast to help restore symmetry. These cosmetic procedures include breast lift, breast reduction, and breast augmentation. If multiple procedures are involved, breast reconstruction may be done in stages.
Timing of Breast Reconstruction
In many cases, breast reconstruction can be done immediately as a part of the mastectomy. Or it can be done later, even years later.
Immediate Breast Reconstruction
There are a number of advantages to immediate breast reconstruction:
- It may be possible to preserve the breast’s skin (known as a skin sparing mastectomy), and possibly the nipple and areola intact (known as a nipple sparing mastectomy).
- Some women have better psychological outcomes with immediate reconstruction: The loss of the breast may be less traumatic because they wake up with a new breast already in place.
- The breast mound may be created at the time of mastectomy and additional procedures still may be necessary.
Delayed Breast Reconstruction
There can be a number of reasons for delaying reconstructive surgery:
If you are having a single mastectomy, you may also wish to have cosmetic surgery on the opposite breast to help restore symmetry. These cosmetic procedures include breast lift, breast reduction, and breast augmentation. If multiple procedures are involved, breast reconstruction may be done in stages.
- Radiation, if needed, may change the appearance of the new breast, as it can create a loss of volume and cause hyperpigmentation. If radiation will be required after mastectomy, the types of immediate breast reconstruction you can have will be limited until treatment is complete and your skin is fully healed.
- If radiation is needed, it may result in additional stages of reconstruction. A tissue expander may be required as an interim stage until radiation is complete.
- You may want to postpone your decision about breast reconstruction until you’ve completed your cancer treatment.
- Other medical issues, such as morbid obesity, active smoking, and pregnancy, may also be deciding factors in delaying your breast reconstruction.
There are some disadvantages to delayed reconstruction as well:
- The skin, nipple and areola from the original breast will no longer be available and can’t be used as part of the reconstruction.
- Delayed reconstruction requires additional surgeries.
Common Concerns
about Breast
Reconstruction
Breast reconstruction is a complex procedure, and it’s natural to have concerns about the process and what you can expect afterward. Here are answers to some common questions:
Will my oncologist be able to detect breast cancer recurrence after having breast reconstruction?
Fortunately, in the vast majority of cases, the answer is yes. The majority of recurrences are just beneath the skin and therefore are palpable and tend to be found in imaging as part of routine ongoing cancer screening.
Does breast reconstruction make breast cancer recurrence more likely?
Studies have shown that reconstruction does not increase the chances that breast cancer will come back. Though certain types of textured breast implants are linked to a rare type of cancer called anaplastic large cell lymphoma (ALCL), our surgeons no longer use this type of implant.
Is breast reconstruction covered by insurance?
Under the Women’s Health and Cancer Rights Act of 1998 (WHCRA), insurance companies are required to pay for breast reconstruction after a mastectomy or lumpectomy. The WHCRA also includes surgery of the unaffected breast to achieve balance and symmetry. The WHCRA covers implant-based reconstruction as well as natural tissue reconstruction, and it is not affected by the timing of your reconstruction, whether immediate or delayed. Learn more about insurance coverage for breast reconstruction.
Talk with Your Surgeon
If you decide you’d like to have breast reconstruction, talk openly to your plastic surgeon about your preferences and concerns. Your surgeon will evaluate your medical history and health, let you know what options are available to you, and explain the benefits and disadvantages of each.
Here are some factors to think about and discuss:
- Do I want surgery on just the cancer breast or on both breasts?
- What size and shape do I want for the new breast?
- Can skin from the original breast be used for the new breast?
- Can the nipple and areola from the original breast be used for the new breast?
- Do I mind having an implant in me?
- If I’m considering natural tissue reconstruction, do I mind having a secondary donor site scar?
- If I need chemotherapy treatment or radiation therapy, how will that affect the breast reconstruction process?
- Does my medical history (including smoking, diabetes, high blood pressure, and obesity) increase my risk for certain types of breast reconstruction?