Lymphedema Overview
Lymphedema can be a difficult complication of breast cancer.
Fortunately, there are options for preventing this condition.
Lymphedema can develop secondary to breast cancer surgery or radiation treatment.
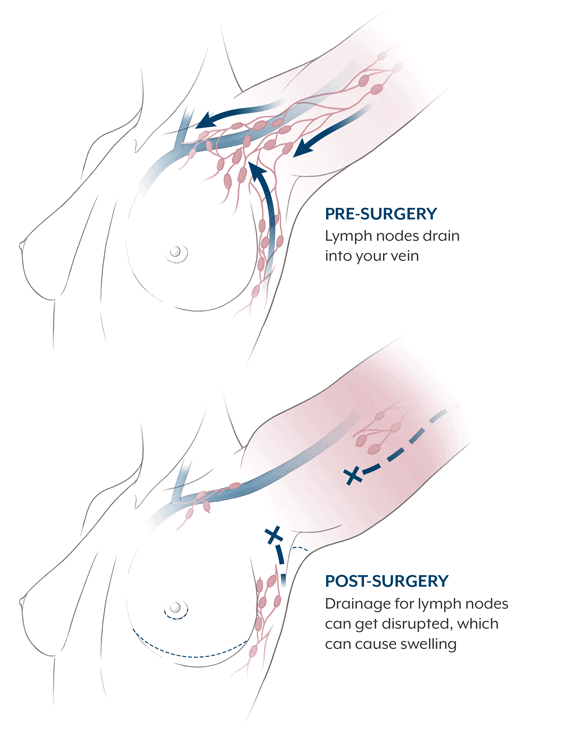
Lymphedema often occurs when lymph nodes in the armpit (axillary) area are removed or damaged as part of cancer treatment. As a result, there may be compromise or blockage in the lymphatic system that creates abnormal swelling. The swelling may appear in the hand, arm, breast, or torso, and can happen months or even years after your treatment. In severe cases, lymphedema can be painful and may limit your movement, interfering with your daily activities. There’s no way to know for certain if you’ll have lymphedema after your breast cancer treatment, but there are factors that make it more likely.
Lymphedema is not considered curable. Conservative methods of treatment, such as compression techniques and manual lymphatic drainage, may be helpful in controlling symptoms but are not always effective.
Recently there has been a shift to preventing lymphedema before it occurs. LYMPHA is a cutting-edge, risk-reducing procedure that has proven successful at lymphedema prevention. The Friedman Center is proud to be one of the few centers in the world to perform this innovative technique.
The Lymphatic System
To understand the condition of lymphedema, and what steps may be taken to help prevent it, you need to know a bit more about the body’s lymphatic system.
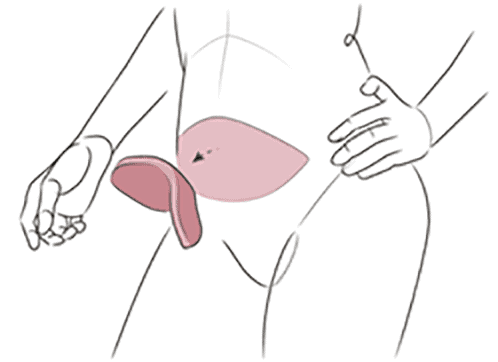
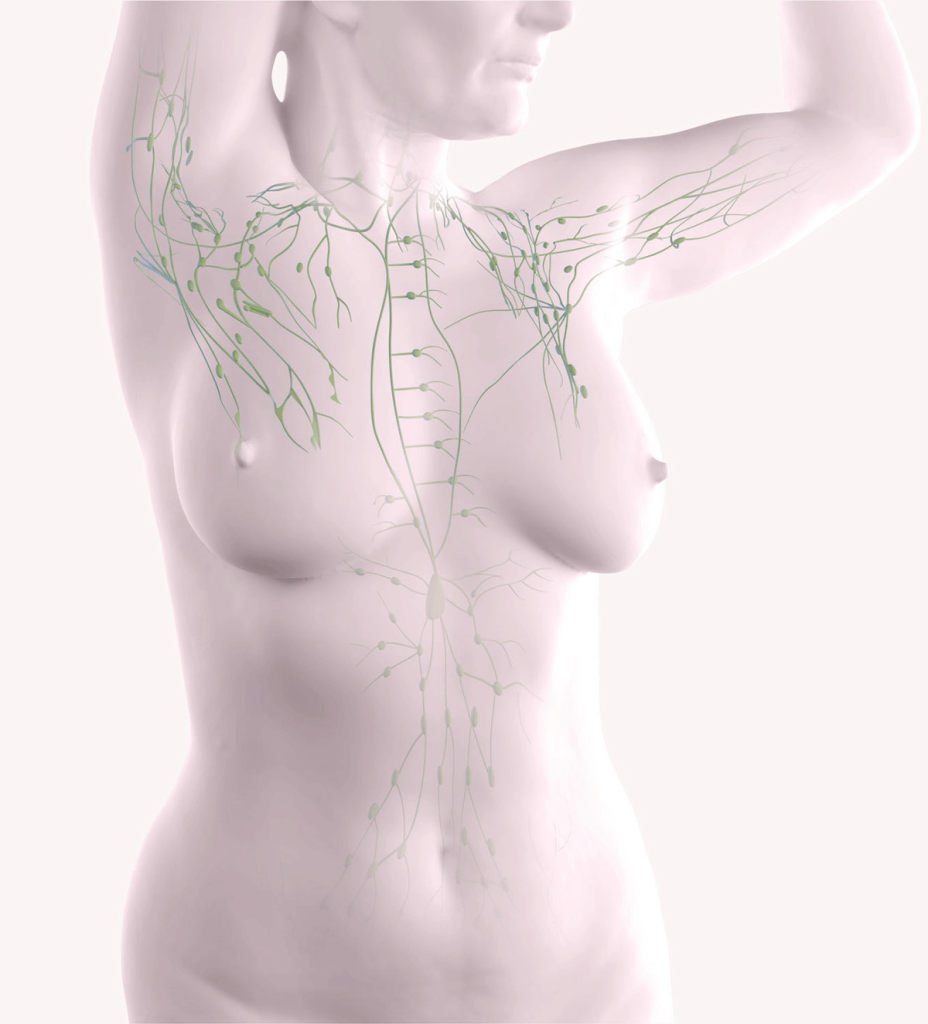
The lymphatic system is similar to your body’s blood circulatory system, consisting mainly of vessels that branch through all parts of the body. The vessels carry a colorless fluid called lymph. Lymph carries white blood cells, a key component of the immune system. As lymph circulates throughout the body, it leaks out into the body’s tissues. There it collects bacteria, dead cells, waste products, and—if they are present—cancer cells. Then, lymph flows back into the lymph vessels and is transported to the lymph nodes.
Lymph nodes are small, bean-shaped structures that filter out bacteria, damaged cells, and other waste from lymph. Lymph nodes are found in many parts of your body, including your groin, neck, pelvis, and underarm (axillary) area, near your breast.
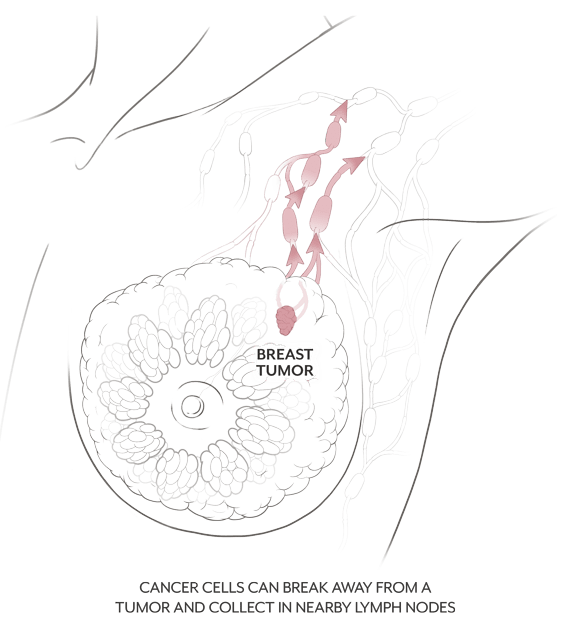
Breast Cancer and the Lymph Nodes
That’s why doctors examine the lymph nodes nearest to your breast when they’re looking to see if breast cancer has spread. In a procedure called a sentinel node biopsy, two or three nodes may be removed for examination. If cancer cells are present, you may need an axillary node dissection, in which up to 30 lymph nodes may be removed.
Surgery, radiation treatment, and extensive dissection can all damage the axillary lymph nodes and lymph vessels. The remaining, undamaged lymph nodes and vessels then have to take over the job of carrying and filtering lymph. If the remaining lymph nodes become overloaded, lymph backs up into the body’s tissues, often into the arm. This backup of lymph, and its resulting swelling, is called lymphedema.
Early Symptoms of Lymphedema
Lymphedema may develop in the weeks or months following surgery or radiation treatment. It can affect your axillary area, hand, arm, chest, or breast. Early signs of lymphedema may be tingling or numbness, which you may experience before any swelling is visible. You may also have sensations of achiness, fullness, or heaviness as well as decreased flexibility at the affected joint. The skin of your arm may thicken and harden. If you notice any of these symptoms, tell your doctor.
Early Treatment of Lymphedema
It’s important to start treating lymphedema early. Consult with a lymphedema therapist who may recommend Complete Decongestive Therapies (CDT) that include Manual Lymphatic Drainage (MLD), movement exercises, bandaging and/or wrapping, and compression garments.
The Lymphedema Surveillance program at Northwell Health utilizes advanced biomedical technology to assist with early detection of lymphedema and ongoing monitoring of treatment. Our physicians use noninvasive bioimpedance spectroscopy (BIS) device to aid in the assessment of secondary lymphedema and to deliver a precise snapshot of fluid status and tissue composition in less than 30 seconds.
DOWNLOAD for more information.
Risk Factors for Lymphedema
Although it’s impossible to predict who’ll get lymphedema, it’s known that certain risk factors make it more likely:
Larger Number of Lymph Nodes Removed
Axillary dissection carries a greater risk than sentinel node biopsy because more lymph nodes are removed. According to recent studies, the risk of developing lymphedema after sentinel node biopsy ranges from 3-10%, compared with 20-53% of those who have axillary dissection.
Chemotherapy
Chemotherapy uses certain chemotherapeutic agents, such as taxanes, that may increase the risk of developing lymphedema.
Radiation Treatment
Chemotherapy uses certain chemotherapeutic agents, such as taxanes, that may increase the risk of developing lymphedema.
Obesity or Being Overweight
Obesity is a risk factor for developing lymphedema. Lymphedema can also be exacerbated by weight gain.
Injury or Infection
Obesity is a risk factor for developing lymphedema. Lymphedema can also be exacerbated by weight gain.
Air Travel
Obesity is a risk factor for developing lymphedema. Lymphedema can also be exacerbated by weight gain.
Learn more about your options