Treatment Overview for Breast Cancer » Mastectomy & Lumpectomy
Mastectomy & Lumpectomy
On this page
On this page
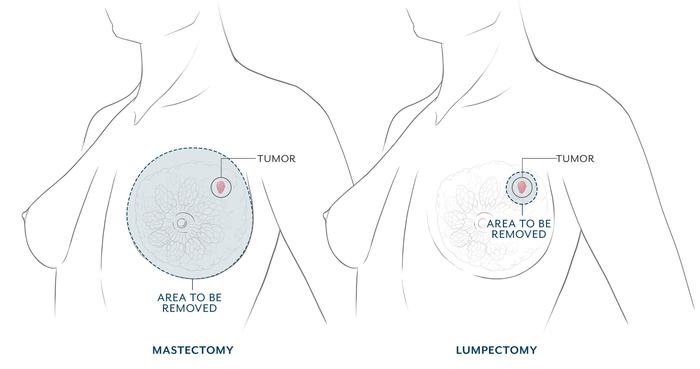
Mastectomy is the surgical removal of the entire breast. A mastectomy may be done as part of breast cancer treatment, or it can be done electively to reduce the risk of developing breast cancer from happening in the future. Women who are high-risk or are genetically predisposed to breast cancer sometimes have a risk-reducing double mastectomy, in which both breasts are removed.
Mastectomy is often done when the tumor is large or involves more than one part of the breast. It also may be done if radiation treatment is not an option. Mastectomy was the original surgery offered for breast cancer. Because it removes nearly all breast tissue (approximately 98%), it is an effective way to obtain local control of many breast cancers.
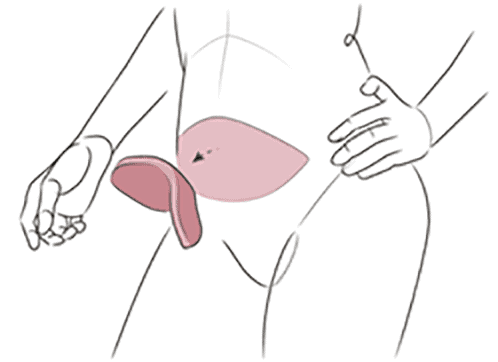
Lumpectomy is often recommended for women with early stage cancers who will receive radiation and have adequate breast tissue volume. A lumpectomy procedure, also called breast conservation surgery or partial mastectomy, involves removing only the portion of the breast that has the tumor along with an adequate margin of normal tissue. Lumpectomy may be done when the tumor is smaller and the breast is larger. Radiation treatment is usually given after lumpectomy to reduce the risk of a cancer recurrence in the remaining breast tissue. Breast surveillance imaging is required after lumpectomy but usually not after mastectomy.
Determining factors for your mastectomy
What Determines the Kind of Mastectomy You Have?
Your doctor will weigh a number of different factors when determining the best type of treatment for you, including: tumor size, breast size, genetic risk, age, ability to receive radiation and overall health. Over the years, an improved understanding of breast cancer progression, improved screening and early cancer detection, more targeted therapies, and the ability to perform immediate breast reconstruction have all led to a decreased need for mastectomy. In some cases, women choose mastectomy over lumpectomy rather than live with the fear of breast cancer recurrence.
Mastectomy vs. Lumpectomy
If you have an early-stage (stage 1 or 2) cancer that hasn’t spread, you may be able to choose between having a lumpectomy or a mastectomy. This decision is a highly personal one.
A large number of studies have shown that women who have mastectomies have the same survival odds as women who have lumpectomies with radiation treatment. But there are many other factors to consider in choosing between mastectomy and lumpectomy.
Many women decide to have a lumpectomy because they want to preserve as much of their own natural breast tissue as possible. They may not want to have complete breast reconstruction and the longer recovery period that comes with it. And, with lumpectomy the chances are good that you’ll retain sensation in the breast. With mastectomy, nerve sensation is lost; partial sensation may return in one to two years.
But bear in mind that radiation treatment is almost always done after lumpectomy. Radiation changes the look and feel of the breast tissue and the breast skin, and it can leave scar tissue. Radiation treatment may create harmful side effects and create long-term problems. If you have a lumpectomy, ongoing surveillance (such as MRIs, ultrasound, mammograms, and breast exams) is still required. Lumpectomy can change the size of the breast and leave dents or distortions in its shape. Partial breast reconstruction may be necessary to restore the shape of the breast.
A lumpectomy can typically be performed as an outpatient procedure, but there may be additional steps required. If the lesion cannot be felt easily, it must first be located through a separate procedure that involves imaging and placement of a special localization seed. After the lumpectomy, your surgeon will receive a final pathology report. If the pathology report finds cancerous cells on the edge of your sample, you may need repeat surgery, known as a re-excision, to remove additional tissue and obtain clear margins.
Advantages & limitations of each surgery
Choosing Between Mastectomy & Lumpectomy
Mastectomy might be a good choice for you if:
- You’ve had radiation treatment to the breast before
- A previous lumpectomy didn’t remove the cancer entirely
- You have dense breasts and imaging surveillance is difficult
- The tumor is large (more than 5 cm [2 inches] in diameter)
- Your breast is small and a lumpectomy will result in distortion of your breast
- You have a genetic predisposition, such as a BRCA mutation, making it more likely you’ll develop cancer in the same or the opposite breast
- You want to avoid ongoing surveillance (such as annual screenings) and the anxiety that often accompanies it
Lumpectomy might be a good option for you if:
- The tumor is less than 5 cm [2 inches] in diameter
- You want to retain as much breast tissue as possible
- You want to preserve sensation in the breast
- You don’t want to undergo complete breast reconstruction
- You would like to have a shorter recovery time than with mastectomy
- Your breast is large enough that the lumpectomy won’t impact symmetry in relation to the opposite breast
Breast cancer can spread from the breast into the lymph nodes in the underarm area. During the mastectomy, surgeons typically take one or more lymph nodes and have them biopsied to see if any cancer is present. If cancer is found, most or all of the lymph nodes will be removed as a part of the mastectomy. This can sometimes result in chronic swelling, a condition called lymphedema.
Fortunately, it’s now possible to perform lymphatic reconstruction to prevent lymphedema at the same time as lymph node removal. The Friedman Center is one of the few centers in the world to perform a cutting-edge surgical intervention for lymphedema prevention, a procedure known as LYMPHA (Lymphatic Microsurgical Preventive Healing Approach).

Talk With Your Surgeons
Breast mastectomy combined with breast reconstruction is a team effort that involves both a breast surgeon and a plastic surgeon. Plan on discussing the process with your surgeons before the mastectomy takes place, even if you’re going to have breast reconstruction at a later date. This allows them to coordinate and plan the best treatment for you.
Additional Treatment After Mastectomy
It’s possible you’ll need additional cancer therapy after mastectomy, but this depends on your individual case. Other therapy might include radiation treatment, chemotherapy, targeted therapy, or hormone therapy. Additional outpatient surgeries may also be needed to complete your reconstruction in achieving your desired result. Consult with your doctor to see if you’ll require additional treatment after mastectomy.