Support Center » FAQs
Frequently Asked Questions
-
All our physicians at the Friedman Center are experienced plastic surgeons who are board-certified by the American Board of Plastic Surgery.
-
Your surgery will take place in one of the Northwell Health hospitals on Long Island, NY. The Friedman Center is a Physician Partner of the Northwell Health system, giving you access to a full spectrum of resources and services before and after surgery.
-
Your core team at the Friedman Center usually includes your plastic surgeon, physician’s assistant or nurse practitioner, and surgical coordinator. We will work closely with the rest of your team, which may include: breast surgeon, medical oncologist, radiation oncologist, primary care physician, genetic counselor, gynecologist, breast nurse navigator, physical therapist, and more.
-
Yes. Under the Women’s Health and Cancer Rights Act of 1998 (WHCRA), insurance companies are required to pay for breast reconstruction after a mastectomy or lumpectomy. You may, however, be subject to copays or deductibles. Check with your insurance company and your physician’s surgical coordinator to confirm coverage and costs.
-
Yes. Our Program Care Coordinator can connect you with other women who are on a journey similar to yours. Visit our Events page to see other opportunities for connecting, including support groups. You can also contact patient advocacy here. You can also hear from women who have had surgery with our physicians.
-
In many cases, breast reconstruction can be done immediately as part of a mastectomy. Or it can be done later, even years later. Timing depends on various factors, including whether you need radiation and if you have underlying medical issues. Your physician can offer further guidance based on your individual circumstances.
-
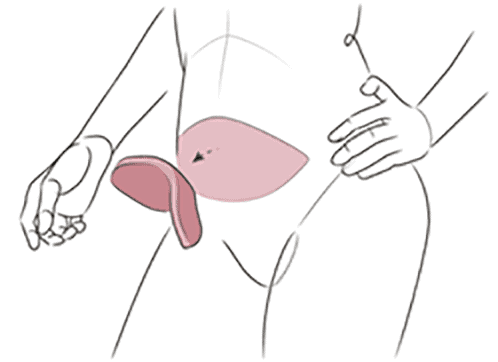
Using your own tissue for breast reconstruction provides the most natural look and feel of any type of breast reconstructive surgery. Your body shape and anatomy may affect the types of breast reconstruction likely to give you the best results.
-
Women who have had prior abdominal surgery, such as a caesarean section (c-section), may still be candidates for DIEP flap surgery. Your physician will be able to evaluate you and discuss your options during your consultation.
-
Yes, you can have breast reconstruction even if you need radiation. The timing differs from patient to patient. You may be a candidate for immediate reconstruction, or your doctor may recommend a staged or delayed reconstruction while you are undergoing treatment or until treatment is complete. Your team at the Friedman Center will coordinate with your oncologist to determine the best treatment plan for you.
-
Many women like the idea of a nipple-sparing mastectomy, in which your native nipple and areola are preserved, and the breast skin envelope and nipple are left completely intact at the time of mastectomy. Nipple-sparing mastectomy is an option for women who have immediate breast reconstruction and is appropriate for women seeking risk-reducing mastectomy or having a mastectomy for cancer. The decision is based on many factors, including the characteristics of the cancer. Talk to your doctor about your eligibility for nipple-sparing mastectomy.
-
Implants do not last a lifetime. They can reach the end of their lifespan after a period of 10-20 years and they will then need to be surgically replaced. If you develop capsular contracture or the implant gets ruptured, you will need to replace them sooner.
-
Many women considering breast reconstruction decide they want to change their breast size. A breast lift (mastopexy), breast reduction (mammoplasty), or enhancement can be considered at the time of your breast reconstruction. If choosing implants, you may be a candidate to choose a size bigger or smaller than your original breast size.
-
Having a lumpectomy may leave breast defects that affect the look and shape of the breast. The size of the breast may also change in relation to the size of the opposite breast. Partial reconstruction after lumpectomy can correct breast defects and restore balance and symmetry.
-
Using your own tissue provides the most natural look and feel of any type of breast reconstructive surgery. Breast implants have evolved significantly over time and today’s newer implants have a softer feel and come in a variety of shapes and sizes that resemble a natural breast. However, you will experience changes in breast sensation and may not have sensation in your reconstructed breasts at all, and your reconstructed breasts will not be able to produce milk.
-
Yes. We care for many patients who live outside the Long Island, NY area. Visit our travel page for information on getting to and staying near the Friedman Center.
-
Download our Mastectomy Checklist and Guide to Your Upcoming Surgery for complete information on surgery and recovery preparation. You can also view in our Support Center on our Patient Forms & Resources page. You can also contact your physician or surgical coordinator if you have any additional questions.
-
Breast reconstruction often involves more than one procedure. The number of surgeries you will need depends on several health-related factors as well as the choices you make about your own reconstruction. If you have a mastectomy with immediate breast reconstruction, you may only need one surgery. If you have delayed reconstruction, you will have at least two surgeries. In either case, most women have more than one procedure, including additional enhancement procedures to achieve optimal results.
-
With the introduction of the innovative (ERP) Enhanced Recovery Pathway protocol, patients have a faster, smoother recovery than ever. Most patients will stay in the hospital one to two days after surgery and will need to recover for several more weeks at home.
-
Studies have shown that breast reconstruction does not increase the chances that breast cancer will come back.