Treatment Overview for Breast Cancer » Mastectomy & Lumpectomy » Risk-Reducing Mastectomy: BRCA & Hereditary Cancer
Risk-Reducing Mastectomy: BRCA & Hereditary Cancer
On this page
If you have high genetic risk factors or other circumstances that increase your risk for breast cancer, you may want to consider a Risk-reducing mastectomy.
Risk-reducing bilateral mastectomy is elective surgical removal of both breasts to prevent future cancer. Some women choose to have a risk-reducing mastectomy because they’re at increased risk due to carrying the BRCA1, BRCA2, or other breast cancer-related genetic mutations.
Women may also choose the surgery because they have a strong family history of cancer, have been diagnosed with lobular carcinoma in situ (LCIS) and have a family history of breast cancer, or received radiation to the chest before the age of 30. Patients undergoing a single mastectomy on a cancerous breast also have the option to have a risk-reducing mastectomy on the opposite healthy breast at the same time, or any time later. This procedure is known as a contralateral prophylactic mastectomy.
How Effective Is Risk-reducing Mastectomy?
While risk-reducing mastectomy reduces a woman’s risk of developing breast cancer below that of the general population, it is important to note that it does not eliminate your risk completely. That’s because mastectomy doesn’t remove all breast tissue and small remnants of breast tissue may remain after your procedure.
You’ll want to carefully consider the risks and benefits of a risk-reducing mastectomy based on your personal circumstances. Your care team can help you evaluate the options and make the best choice for you.
Should You Consider a Risk-Reducing Mastectomy?
The National Cancer Institute recommends that only women at very high risk of breast cancer have a risk-reducing mastectomy. You might consider the surgery if you:
- Have a strong family history of breast cancer
- Carry BRCA1, BRCA2, or other breast cancer-linked mutations
- Have a history of cancer in one breast and a high risk of getting it in the other
- Have a history of cancer in one breast and have dense breast tissue or calcifications that make breast screening difficult
- Were diagnosed with LCIS and have a family history of breast cancer
- Had radiation to the breast before age 30
Genetic Testing for BRCA Mutations
Women can inherit a genetic mutation that raises the risk of breast cancer from either their mother or their father. The two best-known genes that can mutate and increase breast and/or ovarian cancer risk are BRCA1 and BRCA2.
Women who have a BRCA1 or BRCA2 mutation are five times more likely to get breast cancer than women without those mutations. The BRCA mutations also make ovarian cancer more likely.
Now, we also know there are a number of other genes that are known to influence breast cancer risk. Ongoing research is helping to identify genes other than BRCA1 and BRCA2, including mutations in the PALB2, CHECK2, ATM, BARD1, PTEN, TP53, NF1, CDH1, NBN, and STK11 genes.
If you have a strong family history of breast and/or ovarian cancer, you might carry a genetic mutation and may want to consider genetic testing. You may also want to consider genetic testing if you’re unsure of your family medical history, or if you have been diagnosed with breast cancer, ovarian cancer, or two or more types of other cancers.
Genetic testing involves giving a saliva or blood sample for analysis. See a genetics counselor to learn more. It is important to consult with a specialist in cancer genetics when determining your risk for breast cancer and making risk-management decisions that are best for you.
Breast Reconstruction Options
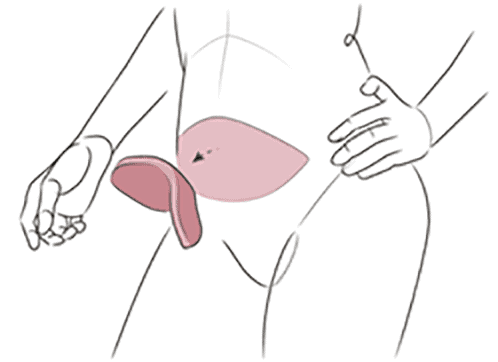
Breast reconstruction can be done during or after risk-reducing mastectomy. If reconstruction is done at the same time as the mastectomy, it’s usually possible to do skin-sparing or nipple-sparing surgery, which removes the breast tissue and almost all of the glands where cancer is most likely to develop but preserves the skin. In some cases, your plastic surgeon may recommend a staged approach, with a breast lift or reduction performed to optimize the breast shape and nipple position prior to the mastectomy, in order to improve the aesthetic outcome.
Learn more about your options for breast reconstruction